Comparing Causes of Maternal Deaths in Two Tertiary Hospitals in Sub-Saharan Countries
Globally, an estimated 585,000 maternal deaths occur annually, with 90% occurring in developing countries, specifically Sub-Saharan African and Asian countries[1]. This makes improving maternal care a major global priority. To achieve this, several interventions and initiatives were implemented across countries such as availability of skilled birth attendants, capacity building sessions, increased antenatal service coverage, and promotion of childbirths with skilled birth attendants. These interventions increased rapidly between 1990 and 2015 with the renewed efforts of the UN to achieve a 75% reduction in maternal mortality by 2015 as the goal 5 of the Millennium Developmental Goal (MDGs). Although a 29% decline in maternal deaths was seen after this period, 289,000 women still die annually due to maternal complications[2]. Available evidence shows that majority of these maternal deaths occurred in a health facility thus, the question of the quality of maternal services delivered[3]. To address the question, a clear understanding of the causes of maternal deaths, associated factors, and emphasis on the type 3 delay is crucial. This write-up reviews the causes of maternal deaths in two tertiary hospitals in two Sub-Saharan African countries (Nigeria and Liberia), and how they compare.
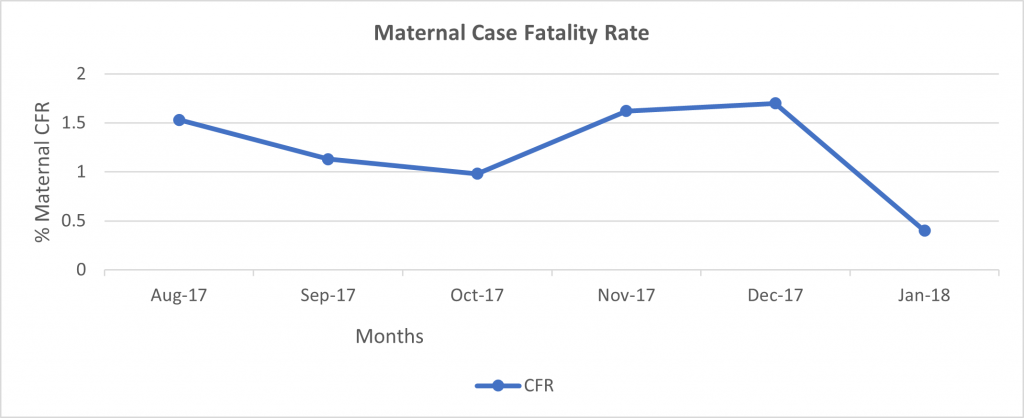
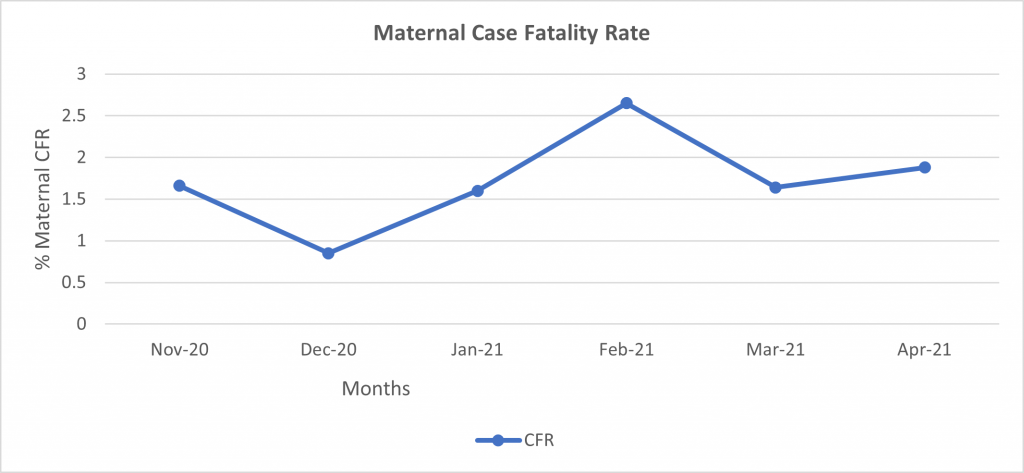
A six-month retrospective review of medical records of all maternal deaths in both tertiary hospitals from August 2017 to January 2018 (for Nigeria) and from November 2020 to April 2021 (for Liberia) was conducted. In the Nigerian hospital, a total of 1,685 deliveries took place, and 21 maternal deaths were recorded during the review period. This gives an average maternal facility case fatality rate of 1.25% (see figure 1 below). The three major direct causes of maternal deaths were Eclampsia (57%), Hemorrhage (10%), and Sepsis (10%). Furthermore, most (90%) of these maternal deaths were unbooked patients and infers a relationship between antenatal care and maternal outcome. In the Liberian hospital, during the review period, 2,171 deliveries and 40 maternal deaths were recorded. Therefore, the average maternal case fatality rate was 1.84% (see figure 2 below). The major drivers of direct causes of maternal deaths were Hemorrhage (30%), Eclampsia (20%), and Sepsis (18%). However, due to poor documentation, no further details were obtained but interviewed clinicians confirmed that most maternal deaths were unbooked cases.
In both hospitals, indirect causes of maternal deaths were poor health-seeking behavior, financial barriers, cultural beliefs, delayed presentation, and institutional barriers. The institutional barriers which are referred to as type 3 delay include lack of basic equipment and stock-out of life-saving drugs, inadequate number of skilled birth attendants, poor uptake and adherence to protocols/guidelines, and lack of emphasis on patient-centered services.
Therefore, a holistic approach that prioritizes both inputs and the implementation of a quality initiative targeted at addressing these barriers will result in a decline in maternal mortality. An approach that entails system thinking, stakeholder engagement, capacity building, application of the model for improvement, performance management, and procurement of required input will result in a reduction in facility-based maternal deaths. Utilizing the holistic approach described above within a period of 30 months (February 2018 – July 2020) in the Nigerian tertiary hospital resulted in a decline of facility-based maternal deaths. Based on learnings in the Nigerian hospital, the approach is being scaled up in the Liberian hospital, which has a similar context over a shorter period (12 months).
Source:
[1] Reduction of Maternal Mortality. Joint WHO/UNFPA/UNICEF/World Bank Statement. Geneva 1999
[2] Kassebaum NJ, Barber RM, Bhutta ZA, et al. Global, regional, and national levels of maternal mortality, 1990–2015: a systematic analysis for the global burden of disease study 2015. Lancet 2016; 388:1775–812.
[3] Countdown to 2030 Collaboration. Countdown to 2030: tracking progress towards universal coverage for reproductive, maternal, newborn, and child health. Lancet 2018; 391:1538–48.
Grants and Business Development Specialist
We are seeking a highly motivated and experienced Grants and Business Development Specialist to join our organization. The successful candidate will be responsible for identifying funding opportunities, developing grant proposals, and fostering partnerships with potential donors and stakeholders (regional and global). This role plays a vital part in securing funds and resources to support our organization’s mission and projects.
Apply NowPublic Health Consultant, Guinea
The consultant (working with the Accelerator team) will collect results from the tool, organize a meeting with stakeholders to discuss results from the tool, and produce a report on key findings and recommendations from the tool to be shared publicly.
Apply NowPublic Health Associate, Senegal
We are currently in search of an experienced Public Health professional in Senegal to work on the anticipated Nutrition Capacity Development and Financing Platform and provide technical assistance to elevate nutrition financing and strengthen local capacity to support these efforts. The Associate must be bilingual (English and French).
Apply Now